Mold biotoxicity is the inability to process and detoxify mold toxins that genetically susceptible individuals are exposed to via skin contact, inhalation, or digestion.
Mold biotoxicity illness is also known as Chronic Inflammatory Response Syndrome. According to research, genetically susceptible individuals make up almost 25% of the population.
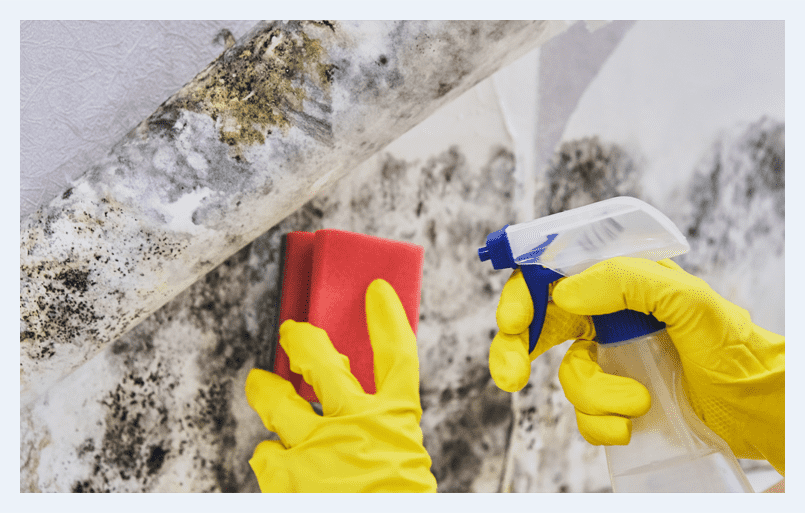
Human beings are exposed to hundreds of thousands of mold species daily, and not all of them are mycotoxins. When indoor molds grow without competition from their natural environment, clinical manifestations are seen in patients with sick building syndrome. Water vapor production occurs in rooms like the kitchen, laundry room, and bathroom. The vapors in these rooms then condense on cooler surfaces such as windows and walls and lead to the colonization of mold spores.
How Do Mold and Biotoxins Attack the Body?
When biotoxins or mold spores come in contact with the body, the removal is through the normal function of the patient’s immune system. The immune response breaks the biotoxins down and excretes them out of the body. Biotoxins are also removed from the body’s bloodstream by the liver.
If the patient’s genes tend to develop chronic inflammatory response syndrome, ingesting or breathing mold biotoxins illness may have a more complicated effect on the body. The pattern recognizing receptors on the body’s immune system cells typically identify and recognize a threat, stimulating the production of cytokine proteins. These cytokines signal the body’s immune cells to attack that threat.
When a patient is genetically sensitive to chronic inflammatory response syndrome, the biotoxins stay bound to the pattern recognition receptors. The receptors keep telling the body that there’s a threat and a continued production of cytokines goes on. Still, the patient’s immune system is left weak and ineffective because it is continually triggered. The frequent stimulation of the patient’s immune system leads to it attacking other body tissues, leading to inflammation.
An excess of cytokines also results in a drop in the melanocyte-stimulating hormones, producing a hormone imbalance. Chronic inflammatory response syndrome is the body’s effort to respond to the mold biotoxin threat, but it tends to cause more illness than a simple allergy.
Symptoms of Mold Biotoxin Illness
Following are some common symptoms:
Eye/Ear/Nose/Throat Symptoms
- Blurred or hazy vision
- eyes sensitive to light
- night blindness
- ringing in the ears
- hearing loss
- dizziness
- sinus/nasal congestion
- nose bleeds
- sensitive to odors
- vocal cord polyps
- laryngitis or raspy voice
- sore throat
Musculoskeletal Symptoms
- Joint pain
- muscle cramps
- muscle weakness
- tics
- spastic muscles
- charlie horses
- morning stiffness
Lungs/Heart Symptoms
- Shortness of breath and tachycardia
- cough
- wheezing
- asthma
- swelling or edema
- heart palpitations
Digestive/Liver/Urinary Symptoms
- Metallic taste in the mouth
- bile reflux
- nausea
- vomiting
- diarrhea
- abdominal pain
- weight loss
- urinary frequency
Nervous/Endocrine/Immune Symptoms
- Insomnia
- headache
- mental confusion
- poor concentration
- poor short-term memory
- extreme thirst
- low blood pressure
- reduced body temperature regulation
- numbness
- tremors
- vertigo
- Parkinson’s-like symptoms
- anxiety
- swollen and painful lymph nodes
Standard Testing for Mold Biotoxin Illness
In mold biotoxin illness If chronic inflammatory response syndrome is presumed, a blood test is conducted to check for HLA-DR and HLA-DQ genes, indicating CIRS susceptibility. Testing is carried out for high amounts of cytokine in the patient’s blood along with marked differences in levels of the following hormones and antibodies:
Vasoactive Intestinal Peptide
This hormone is responsible for controlling the absorption of water and electrolytes in the body’s gut. It is also responsible for heart and vascular functions. Low levels of the vasoactive intestinal peptide can cause watery diarrhea and indicate Chronic inflammatory response syndrome.
- Transforming Growth Factor-beta 1
It is a specific type of cytokine responsible for cell division and death. Large numbers indicate Chronic inflammatory response syndrome and shortness of breath.
- Melanocyte Stimulating Hormone
Also known as MSH, this hormone controls the pigment of the body’s skin and how many cytokines the body will produce. Low levels indicate chronic inflammatory response syndrome, as the body cannot shut down cytokine production.
- C4A
These are a part of the complement group comprising proteins that work with the patient’s immune system. They are responsible for stimulating neutrophil cells, which can worsen inflammation. Large numbers of C4A can indicate Chronic inflammatory response syndrome.
- Adrenocorticotropic Hormone (ACTH)
ACTH usually regulates the body’s cortisol levels. These ACTH levels may initially be high and then reduce when symptoms are more prevailing.
- Cortisol
This hormone has many different functions but is released in higher quantities when the body is stressed, or the immune system needs backup. Cortisol levels may be high at the beginning but then drop over time.
- Anti-gliadin Antibodies (AGA) IgA/IgE
These antibodies are created in response to gliadin. Usually triggered if the patient has gluten sensitivity, but they are also affected by mold biotoxins.
- VEGF
Vascular Endothelial Growth Factor causes the formation of blood vessels. Chronic inflammatory response syndrome patients typically show a deficiency in VEGF.
- Leptin
Leptin hormone helps control fat storage in the body. High leptin levels result in quick, easy weight gain, another signifier of chronic inflammatory response syndrome.
Anti-cardiolipin antibodies (ACLA) IgA/IgG/IgM –
Patients with autoimmune disorders have Anti-cardiolipin antibodies. Increased numbers usually indicate that the body is dealing with great levels of inflammation. The antibodies are often attacking the body’s healthy tissues instead of the biotoxins.
How is Mold and Biotoxin Disease Treated at Silver Cancer Institute and Cancer Center for Chronic Disease?
Personalized Genomic Treatment
Immunodeficiency is present in patients with mold and biotoxin disease. The critical importance of this therapy is to evaluate and restore immune function. Many other conditions are related to mold and biotoxin disease patients, such as Lyme disease, HHV-6, Epstein-Barr, and herpes virus CMV.
The treatment of virus and Lyme disease is done with supportive oligonucleotides(SOT). Antioxidants are restored along with the detoxification of heavy metals.
This treatment comprises a synergistic multi model protocol. Various binders, such as activated charcoal, chlorella, and others, are utilized in getting rid of the mold.
Combination Therapy
This treatment plan is multimodal and synergistic. The patient is helped through immune optimization. There is the killing of coexistent infections, toxins, and heavy metals during this treatment. The optimization of nutritional levels, hormones, along supportive oligonucleotides becomes necessary when indicated.
Search terms
- Mold Biotoxin Illness
- Mold Biotoxin disease
- Chronic Inflammatory Response Syndrome
- Cytokines
- Symptoms of Mold Biotoxin Illness
- Testing for Mold Biotoxin Illness
- Anti-cardiolipin antibodies.